
Mycosis of the feet (dermatophytosis) is an infectious disease caused by pathogenic or opportunistic fungi. With mycosis, the skin on the feet peels and is very itchy, and in severe cases, it becomes red and swollen.
Definition of disease
Mycosis of the feet, or dermatophytosis, is an infectious disease caused by a dermatophyte mold. In total, 43 species of dermatophytes are known, 30 of which lead to foot mycosis. Most often this is the fungus Trichophyton rubrum (90%), Trichophyton mentagrophytes, and less commonly Epidermophyton. Foot mycosis is caused more or less often by fungi of the genus Candida and the molds Scytalidium dimidiatum, Scytalidium hyalinum.
All dermatophytes have keratinolytic activity: they are able to dissolve keratin, the fibrous protein that makes up the upper part of human and animal skin. The skin is damaged.
Once on the skin, the fungus is directed to the most vulnerable place - the junction between the cells of the epidermis. There they penetrate inside and begin to actively grow. However, fungi rarely penetrate deeper than the granular layer of the skin. Usually it is limited to the upper, keratinized tissue.
Prevalence of foot mycosis
Skin mycoses, including foot mycoses, are found in all countries of the world. The share of this disease in the structure of all dermatological diseases reaches 37-40%.
At the same time, skin mycoses occur most often - in about 30% of cases.
According to dermatologists, up to 20% of the adult population suffers from foot mycosis. Pathology is found twice more often in men.
Among people over the age of 70, foot fungus is found in almost every second patient - this is explained by the fact that the elderly usually have chronic diseases related to metabolic disorders, as well as vascular pathologies, such as varicose veins.
Infection with foot mycosis usually occurs in families - through direct contact with the skin of an infected person. There are also known cases of infection when sharing clothes, shoes and household items.
The infection usually affects both feet at once and partially spreads to the nail plate. Without treatment, the disease can also affect the skin of the palms - usually on working hands. This condition is called two feet one hand syndrome.
Causes of foot mycosis
Most often, foot mycosis is caused by dermatophyte fungi - Trichophyton rubrum, Trichophyton mentagrophytes and Epidermophyton floccosum. More rarely, the disease is provoked by fungi of the genus Candida (Candida) and mold (Scytalidium dimidiatum, Scytalidium hyalinum).
According to several studies, the share of dermatophytes in the structure of the causative agent of foot mycosis is gradually decreasing. Candida fungus is the focus.
Risk factors for developing foot mycosis:
- violation of personal hygiene;
- sharing shoes (for example, at bowling alleys, skate and ski rental shops);
- visiting public baths, swimming pools, beaches;
- climatic features: the risk of getting the disease is higher in countries with a subtropical and tropical climate - this is due to increased humidity and ambient temperature;
- always wear closed and tight shoes (this happens among military personnel, miners, workers in the textile and metallurgical industry);
- frequent injuries to the toes due to flat feet, calluses, corns;
- non-compliance with hygiene rules during pedicure;
- impaired blood supply to the legs;
- immunodeficiency conditions, including HIV;
- chronic dermatosis;
- obesity;
- diabetes;
- chronic venous insufficiency;
- taking certain medications (systemic glucocorticosteroids).

Symptoms of foot mycosis
The symptoms of mycosis of the feet, as well as the features of the treatment of the disease depend on its clinical form.
Squamous (squamous-hyperkeratotic) form of foot mycosis
In most cases, the causative agent of the squamous form of foot mycosis is the dermatophyte Trichophyton rubrum.
In the early stages of the disease, the patient is disturbed by simple peeling of the skin between the fingers - the scales on the skin are numerous, thin, and silvery. Then, when the disease spreads to the lateral and dorsal surfaces of the legs, characteristic inflammatory ridges appear, and the skin in the affected area thickens. Over time, the patient developed onychomycosis - nail fungus.
Intertriginous form (interdigital) foot mycosis
This form often develops against the background of severe sweating on the feet. This disease affects the space between the fingers and is accompanied by redness, swelling, and maceration (softening and loosening of the skin). Erosion and cracks often form. Many patients report itching, burning, and pain.
Often, simultaneous infection of the skin of the feet with dermatophyte fungi (usually Trichophyton mentagrophytes var. interdigitale) and Staphylococcus aureus bacteria occurs.

Dyshidrotic form of foot mycosis
As a rule, the causative agent of this form of foot mycosis is Epidermophyton floccosum (epidermophyton flaky).
The dyshidrotic form of foot mycosis, as a rule, is more severe and is accompanied by itching and excruciating pain. Blisters with a thick covering form on the skin. Merging, they form a large multi-chambered blister, which, after opening, turns into a moist pink-red erosion and then into a brown crust.
This disease is difficult to treat and often recurs.
The characteristic feature of the dyshidrotic form is damage to the arches of the feet, interdigital folds and the skin of the fingers. The process can then spread to the heel, the lateral surface of the lower leg, and even to the skin below the ankle.
If a bacterial infection occurs, the patient may have a fever and regional lymph nodes will be enlarged. Swelling on the leg is visible, and the skin on it becomes wet. Severe pain makes it difficult for the patient to walk.
Exudative-dyshidrotic form of foot mycosis
Most often, the exudative-dyshidrotic form of mycosis of the feet is caused by the fungus Trichophyton rubrum (red trichophyton).
The skin between the fingers is affected first. Then the process spreads to the surface of the foot, dorsal and lateral, and the nail plate. Blisters and erosions appear on the skin, which are then covered with crusts. The skin becomes wet and may fester.

A suppressed form of foot mycosis
The deleted form was identified by several researchers. It is believed that it occurs a few days after the fungal infection.
The skin in the interdigital folds begins to peel. There may also be some peeling on the soles and sides of the feet. Patients may ignore unpleasant symptoms, but they still infect others.
Acute form of foot mycosis
The acute form of mycosis on the feet is the result of an exacerbation of the dyshidrotic or intertriginous (interdigital) form.
The disease begins acutely: a large number of blisters appear on the skin of the legs and then the feet. Swollen skin. Then a nodule forms on the hand and the lower third of the forearm.
After the blisters open, erosion appears, surrounded by loose fragments of skin. They merge, turning into a wide weeping surface, often with purulent discharge.
The disease is often accompanied by fever, deterioration of the patient's general condition, and sharp pains in the affected hands and feet. Inguinal and femoral lymph nodes are enlarged and painful.
Vesiculobulous (inflammatory) form of foot mycosis
The inflammatory form of foot mycosis is usually identified by foreign authors, often defining it as acute. It can develop from a form of chronic interdigital dermatophytosis.
As a rule, the causative agent of the vesiculobullous form is the dermatophyte Trichophyton rubrum.
Main symptoms: severe itching, skin rash, localized mainly on the soles of the feet, at the base and on the sides of the fingers, on the back of the legs. Swollen areas with blisters on the surface may appear. Bubbles can merge or remain unchanged for a long time - if the tire (top) is thick enough.
Often the nail plate is also involved in the process - onychomycosis develops.
Ulcerative form of foot mycosis
The ulcerative form (in foreign literature it is called in) is one of the complications of foot mycosis, which is caused by the addition of bacterial infection.
Widespread deep purulent ulcers form on the soles of the feet. Patients experience severe pain and, as a result, difficulty walking.
Complications of foot mycosis
Cracks and ulcers on the skin that appear at the site of mycosis are the entrance for bacterial infection. However, it is more difficult to treat such an infection - this is explained by the fact that the fungus produces special substances that increase the resistance of bacteria to drugs.
The most common complications of foot mycosis:
- allergic dermatitis of infectious and drug origin;
- pyoderma - pustular skin disease (cellulitis, lymphangitis, phlegmon, osteomyelitis of the leg bones), which can lead to deep and long-lasting skin wounds;
- plantar warts;
- microbial eczema is a chronic inflammatory disease in which the skin itches and becomes red, and blisters with a liquid form on it;
- a general decrease in immunity and impaired microcirculation in the lower part of the legs (usually develops in patients with diabetes mellitus and varicose veins);
- the spread of the disease to the skin of the hands and nail plates;
- deterioration in the quality of life: in the acute form of mycosis it is difficult to wear shoes, and lymphadenitis leads to fever and poor health.

Diagnosis of foot mycosis
Dermatologists-mycologists deal with the diagnosis and treatment of foot mycosis.
At the appointment, the doctor will assess the condition of the patient's nails, skin, mucous membranes and hair. He will conduct a dermatoscopy - examining the skin under magnification. In parallel with the examination, the specialist will collect anamnesis and ask the patient about his lifestyle, quality of nutrition, household habits and care procedures.
If you suspect athlete's foot, your doctor will order lab tests.
A skin scraping examination will rule out or confirm a fungal infection.
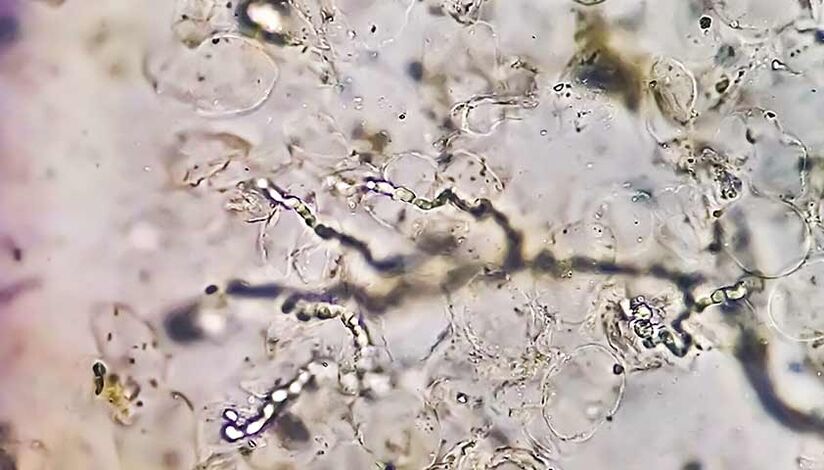
Doctors may also refer patients for microscopic examination and culture.
Sowing, or the culture method, allows you to get more accurate information about the causative agent of the disease, although it takes longer - usually a month.
Diabetes mellitus can worsen the course of foot mycosis and lead to serious complications. A complex study can exclude or confirm this diagnosis.
A complete blood count helps assess the patient's general condition.
Clinical blood tests are blood tests that allow you to assess your general health, identify inflammation, bacterial, viral and fungal infections, and can also help in the diagnosis of anemia, hematopoietic organ diseases, allergic reactions and autoimmune diseases.
Also, before recommending antifungal therapy, the doctor may prescribe the patient a biochemical blood test - this study will determine the level of bilirubin and the liver enzymes ALT and AST. Such information will help the doctor choose the dose of the drug and minimize the risk of side effects.
Treatment of foot mycosis
Treatment of foot mycosis is carried out in two stages.
In the first stageIn case of acute inflammation, lotions are used: aqueous solution of ammonium bitumen sulfonate, an agent with antiseptic properties (Castellani liquid, brilliant green 1% aqueous solution). Then pastes and ointments are prescribed that contain antifungal drugs and glucocorticosteroids.
In the case of severe weeping (in the acute phase) and the addition of secondary infections, anti-inflammatory solutions are used as lotions, as well as combined antibacterial drugs in the form of creams and solutions.
The basis of therapy is the use of antimycotic - antifungal - agents.
At the main leveltreatment using antifungal drugs designed to destroy pathogenic fungi. Most often, such drugs are produced in the form of ointments, creams or solutions.
If the patient is disturbed by severe itching, the dermatologist may prescribe antihistamines. They are usually taken for 10-15 days, until the unpleasant symptoms disappear completely.
When the nail is damaged, an antifungal agent is used - it is applied directly to the nail plate and nail folds. In this case, the drug is concentrated on the surface of the nail and does not penetrate into the bloodstream, eliminating the risk of side effects.
If external drugs do not produce an effect, systemic antimycotic agents are prescribed.
The treatment regimen and drug dosage are determined by the doctor. During treatment, it is necessary to visit a podiatrist at least once a month.
Prognosis and prevention
If you consult a doctor in time, the prognosis for foot mycosis is good: most patients who are treated with antifungal drugs get rid of the disease forever.
To prevent mycosis, you need to protect your feet and hands from irritating and traumatic factors and strengthen your immune system.
Steps to prevent onychomycosis:
- change socks daily or more often if your feet are sweaty or wet;
- shoes air or dry after wearing;
- use an antifungal UV shoe dryer;
- do not wear shared slippers when visiting;
- don't try on shoes in the store with bare feet;
- use a personal towel for your feet;
- use individual tools for nail care (tweezers, files);
- wearing shoes in the swimming pool or sauna;
- monitor the diversity of your diet;
- avoid stressful situations.
Frequently asked questions
How to cure foot fungus?
To treat foot fungus, antimycotic drugs are usually used, which are available in the form of creams, ointments and solutions. Dermatologists should choose the most effective drug and determine the dosage.
Why do my feet itch?
One of the causes of itchy feet is mycosis of the feet, an infectious disease caused by a dermatophyte mold.



























